MEDICAL HIV CONFERENCES AND EVENTS
Each year we attend multiple medical conferences to present our latest research from our innovative pipeline and portfolio of medicines. Although different, each conference plays a key role to ensure continued progress in the HIV response.
2024
3-6th March 2024
CROI
The prestigious Conference on Retroviruses and Opportunistic Infections (CROI) accelerates progress in HIV research. CROI has facilitated the presentation of important discoveries in the field, thereby accelerating progress in HIV research.

22-26th July 2024
AIDS
AIDS is one of the largest medical conference in the HIV calendar, alternating with IAS every year. For physicians, researchers, and the wider HIV community, it's a chance to discover the latest advances in HIV treatment and care.

10-13th November 2024
HIV GLASGOW
HIV Glasgow 2022 is a major medical congress on the HIV calendar. Over the years, HIV Glasgow has been an important congress for scientists and healthcare professionals from around the world to come together to collaborate and share data with the HIV community.

2023
4-9 December 2023
ViiV Healthcare at ICASA 2023
The ICASA conference provides a strong platform for leaders, scientists, activists and community in Africa to come together to advance the HIV response. ViiV Healthcare is proud to be at this event: learn more about our presence at ICASA 2023.

18 - 21 OCTOBER 2023
EACS
The European AIDS Clinical Society Conference (EACS) is an opportunity for the HIV community to come together to discuss the latest in HIV research and how, together, we can continue to support the HIV community.

23 - 26 JULY 2023
IAS Conference on HIV Science
The IAS Conference on HIV Science is the world’s most influential meeting on HIV research and its applications. This biennial conference (alternating with AIDS) presents the critical advances in basic, clinical and operational HIV research that move science into policy and practice.

NP-GBL-HVX-COCO-220058 | February 2024
YOU MAY ALSO BE INTERESTED IN:
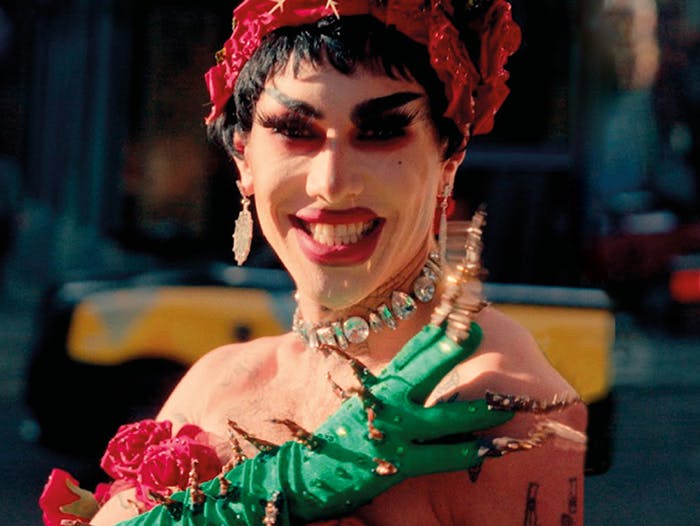
LGBTQIA+ (Lesbian, Gay, Bisexual, Transgender, Queer, Intersex, Ally and anyone else who’s not included) Pride started as a political protest and over the years has become a celebration and acceptance of the self-affirmation, dignity, equality and increased visibility of the community.
World AIDS Day is an annual awareness day, serving as an opportunity for the world to come together to celebrate and support people living with HIV, and at the same time remember those who are no longer with us following AIDS-related illness.
Together we are engaged in the HIV response throughout the world, supported by a team of over 1,100 dedicated ViiV Healthcare staff working across the globe.
If you get any side effects, talk to your doctor, pharmacist or nurse. This includes any possible side effects not listed in the package leaflet. You can also report side effects directly via the Yellow Card Scheme at www.mhra.gov.uk/yellowcard or search for MHRA Yellowcard in the Google Play or Apple App store. By reporting side effects, you can help provide more information on the safety of this medicine.
If you are from outside the UK, you can report adverse events to GSK/ViiV by selecting your region and market, here.