FACING THE CHALLENGES OF AGEING WITH HIV

Advances in treatment have dramatically improved the life expectancy of people living with HIV (PLHIV), which is welcome progress. However, challenges remain for those ageing with HIV.
Michael Dorosh was first diagnosed with HIV in 1990, and in 1995, when he started to experience a rapid decline in health, he believed he only had a year left to live. However, thanks to advances in treatment, he has now been living with HIV for more than half of his life.
Now a long-term survivor and Director of the Treatment Educat10n Network (TEN) in Denver, Colorado, Michael acknowledges that challenges and uncertainties remain when it comes to getting older with HIV, and said “people living with HIV may experience age-related health challenges earlier than usual.”
Significant advances have been made in the development of effective HIV treatments that allow PLHIV to suppress their virus to undetectable levels, shifting the prognosis from a fatal infection to the management of a chronic illness. As a result of these advances, PLHIV increasingly live longer and healthier lives and increasingly can expect to live as long as those who do not have HIV.
Despite notable progress in HIV treatment, challenges remain for those ageing with HIV. Andrew Clark, Global Medical Lead at ViiV Healthcare said, “There are medical challenges for those who become resistant to HIV medicines; adherence challenges for those who have difficulty sticking to daily medication, and the additional pressure of having to manage other medical conditions, known as ‘co-morbidities.’ Additionally, these individuals may also face significant social challenges such as a lack of access to care and experiencing stigma.”
Andrew Clark, Global Medical Lead, explains that we must change the way we approach treatment for people ageing with HIV.
An increasing, ageing population
There has been a dramatic change in the demographics of the population of PLHIV with HIV clinics now caring for an increasing number of people aged 50 years or older. According to the medical journal Lancet HIV, it’s estimated the median age of people on treatment will increase from 44 years in 2010 to 57 in 2030, with the proportion of PLHIV aged 50 years or older increasing from 28% in 2010 to 73% in 2030.1,2
In addition, PLHIV may have an elevated risk of a variety of chronic illnesses so may require additional care, particularly as the population of PLHIV who are ageing grows.3 These statistics point to a growing need for specialised research and care focused on those PLHIV who are ageing, and the chronic conditions associated with HIV.4
The changing treatment needs of older PLHIV
Current novel ARTs allow many PLHIV to achieve a near-normal life span; however, as people age, the risk of other health challenges increases.5 These health challenges include cardiovascular disease, cancer, osteoporosis and other diseases in which the organs, such as the liver or kidney, are ultimately affected by chronic or progressive diseases.6
The general commitment among the scientific community is to design treatment that will have a minimal intrusion on the lives of PLHIV, including a good safety and tolerability profile, with limited organ-related side-effects, or ‘toxicities’ (such as those affecting the liver or kidney) and interactions that occur between different medicines. However, a better understanding of how age affects PLHIV, and how ART may influence this will help address the clinical issues faced by the ageing PLHIV community.
Taking multiple medications creates concerns for PLHIV, one of which, is the impact they might have on the immune system. As we age, so does our immune system, making it more difficult for the body to fight off infection and cancers. The ageing immune system is further impaired by HIV-associated complications, causing ongoing inflammation.
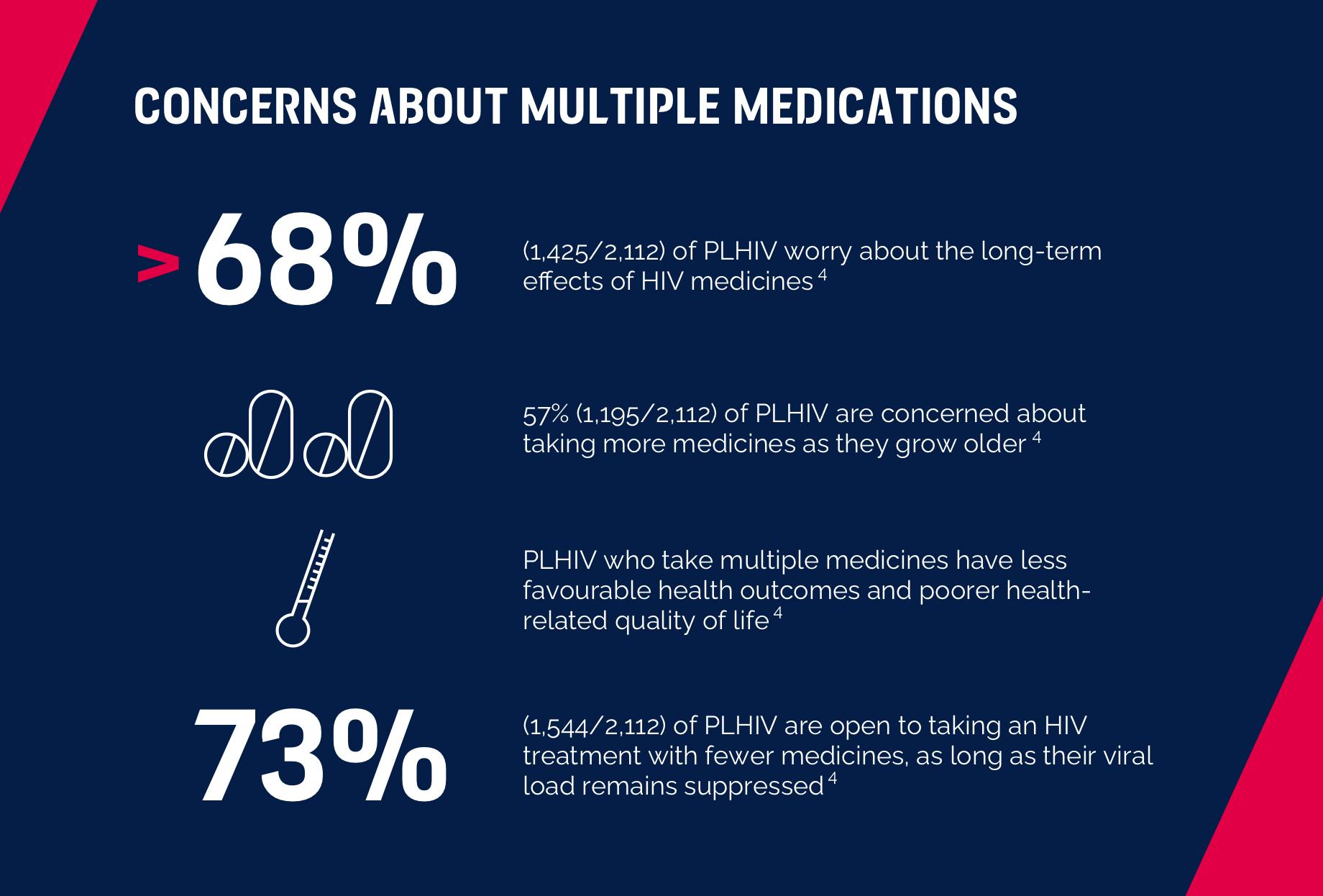
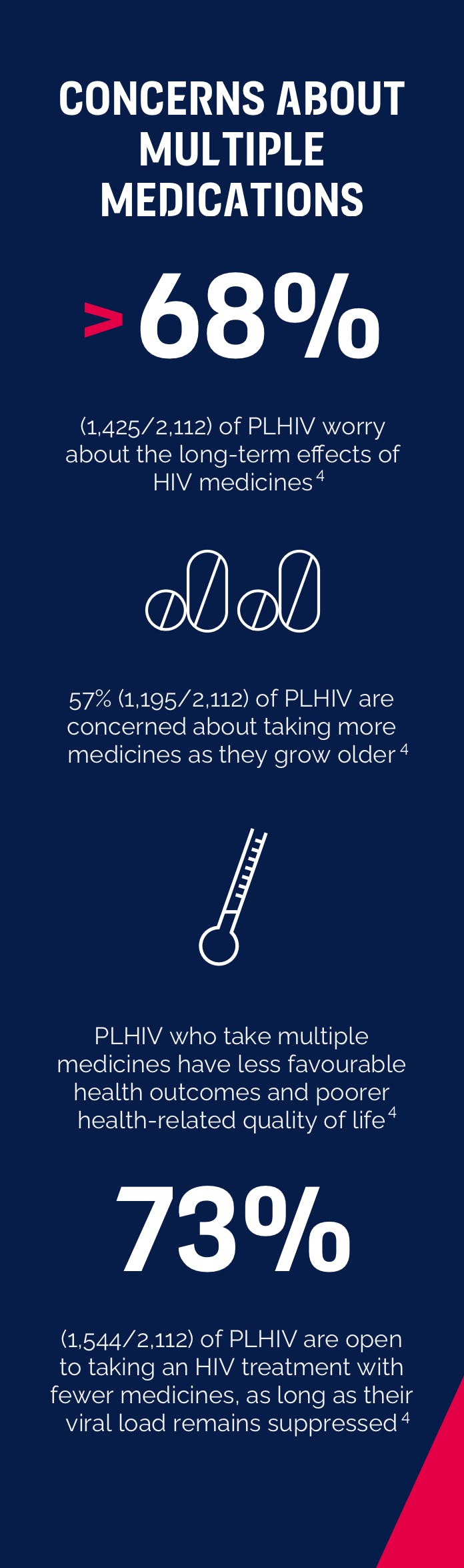
Sponsored by ViiV Healthcare and developed in collaboration with an international, multi-disciplinary Advisory Committee, findings from the Positive Perspectives Study suggests that PLHIV are concerned about taking multiple medications.7
Michael Dorosh notes that our immune systems evolved over millions of years by fighting pathogens then going into rest. When our immune system fights, it leads to inflammation.
“What we discovered was that even though your virus might be undetectable, your immune system is still fighting something 24/7, and that might be one of the reasons why people living with HIV may experience health challenges earlier than usual.” – Michael Dorosh, Director of the Treatment Educat10n Network (TEN).
Scientists are looking into multiple sources and studies to better understand ageing in PLHIV and are investigating the potential therapeutic treatments or interventions that could be combined with ART to improve outcomes for PLHIV.
What about stigma?
While ART and HIV management has continued to improve, social and health consequences of stigma have persisted and, in many countries, increased. As Michael Dorosh notes, “HIV is now a treatable chronic disease with few complications, but the disease we have no treatment for is stigma.”
"HIV is now a treatable chronic disease with few complications, but the disease we have no treatment for is stigma."
Stigma against the elderly adds to the existing multifaceted HIV stigma, potentially denying older PLHIV access to optimal care and a healthy social environment. The American Psychological Association says this may be a result of a rejection by social network members or self-protective withdrawal and can lead to loneliness and depression.8
Data presented at the AIDS 2020 conference highlight how stigma remains an issue for some PLHIV as they grow older. During the conference, researcher Han Siong Toh shared results from a standard questionnaire measuring HIV stigma and discrimination among health facility staff in Taiwan, which showed that further education is still necessary, not only to staff new to working in HIV but also to those already working in the field.9 Jeffrey Hirono from HIV Scotland has highlighted the need for more research on the connection between ageism and HIV-related stigma, and the link between mental health and financial insecurity among older PLHIV.10
Mapping a new future in HIV
ViiV Healthcare is committed to helping PLHIV live long, healthy lives. We run and support multiple studies to build our understanding of how treatments affect older PLHIV.
“We need to understand the unique contribution that HIV is making to the ageing process for PLHIV. To better understand this phenomenon, long-term follow-up from large patient groups who are both HIV positive and HIV negative will provide insights on management and prevention.”
We are working to help understand the clinical, scientific and societal effects of HIV on ageing. Our research programmes focus on generating meaningful data for new medicines and treatment strategies, with the aim of reducing the short and long-term burden of ART on the lives of PLHIV. This involves close engagement with patient organisations, including educational programmes and data generation.
In a recent trial for one of our investigational medicines, at least 25% of PLHIV enrolled were aged 50 years and over. We also actively support and are involved in large observational studies in older PLHIV, such as the POPPY (Pharmacokinetic and clinical Observations in People over fifty) cohort and ADHOC (Aging with Dignity, Health, Optimism, & Community) cohort. These are studies that not only look at the clinical challenges faced by PLHIV, but also societal factors that may impact their wellbeing.
By collaborating with the community that is directly impacted by these issues, we are supporting efforts that improve the care and control of the HIV epidemic helping us to map a new future in HIV, leaving no person living with HIV behind.
References
- AIDS info. Available at: http://aidsinfo.unaids.org/. Accessed August 2020
- Smit et al., Lancet Infect Dis 2015 Jul;15(7):810-8). Global AIDS Update. Available at: https://aids2020.unaids.org/report/. Accessed August 2020
Yang H-Y, et al. Scientific Reports 2019;9:18514 - UNAIDS. The Gap Report. Available at: http://www.unaids.org/sites/default/files/media_asset/UNAIDS_Gap_report_en.pdf. Last accessed: Nov 2016
- Smit M, Brinkman K, Geerlings S, et al. Future challenges for clinical care of an ageing population infected with HIV: a modelling study. Lancet Inf Dis 2015;15:810-18.
- Gebo KA. Epidemiology of HIV and response to antiretroviral therapy in the middle aged and elderly. Aging Health 2008; 4: 615–27
- Okoli C, de los Rios P, Eremin A, Brough G, Young B, Short D. Relationship Between Polypharmacy and Quality of Life Among People in 24 Countries Living With HIV. Prev Chronic Dis 2020;17:190359. DOI: http://dx.doi.org/10.5888/pcd17.190359
- Nobili A. Multiple diseases and polypharmacy in the elderly: challenges for the internist of the third millennium. J Comorbidity 2011; 1:28–44
- Toh HS, et al. AIDS 2020. PED0830
- Hirono J. AIDS 2020. PED0785.
YOU MAY ALSO BE INTERESTED IN:
Incredible advances have been made in the development of effective HIV treatments that allow people living with HIV to suppress their virus to undetectable levels and avoid transmitting it to others. Find out about our approach to HIV cure.
Today, out of all the key populations affected by the HIV epidemic, women make up more than half (52%) of all people living with HIV worldwide and HIV/AIDS is now the leading cause of death globally for women aged 15-44.
If you get any side effects, talk to your doctor, pharmacist or nurse. This includes any possible side effects not listed in the package leaflet. You can also report side effects directly via the Yellow Card Scheme at www.mhra.gov.uk/yellowcard or search for MHRA Yellowcard in the Google Play or Apple App store. By reporting side effects, you can help provide more information on the safety of this medicine.
If you are from outside the UK, you can report adverse events to GSK/ViiV by selecting your region and market, here.

