UNDERSTANDING HIV AND TUBERCULOSIS CO-INFECTION

For people living with HIV who also have tuberculosis (TB), it’s called an HIV and TB co-infection.
While co-infections exist across different conditions, TB is the most prominent in people living with HIV (PLHIV), accounting for 340,000 deaths – approximately one-third of deaths - in 2016; making it the leading cause of death among PLHIV.1
This is largely due to the impact of the HIV virus in weakening the immune system, which increases the risk of contracting TB for PLHIV by 26 times relative to the general population.2 In addition, 54% of TB cases in PLHIV remain undiagnosed.3

These numbers highlight the importance of fighting both HIV and TB together – rather than in isolation. This case is even stronger in regions where the prevalence of TB – and HIV/TB co-infection - is high.
For the medical and scientific communities, who are tasked with developing the next generation of antiretroviral (ARV) therapies for PLHIV, it’s clear that HIV/TB co-infection should be a key consideration.
The disproportionate burden of HIV/TB co-infection
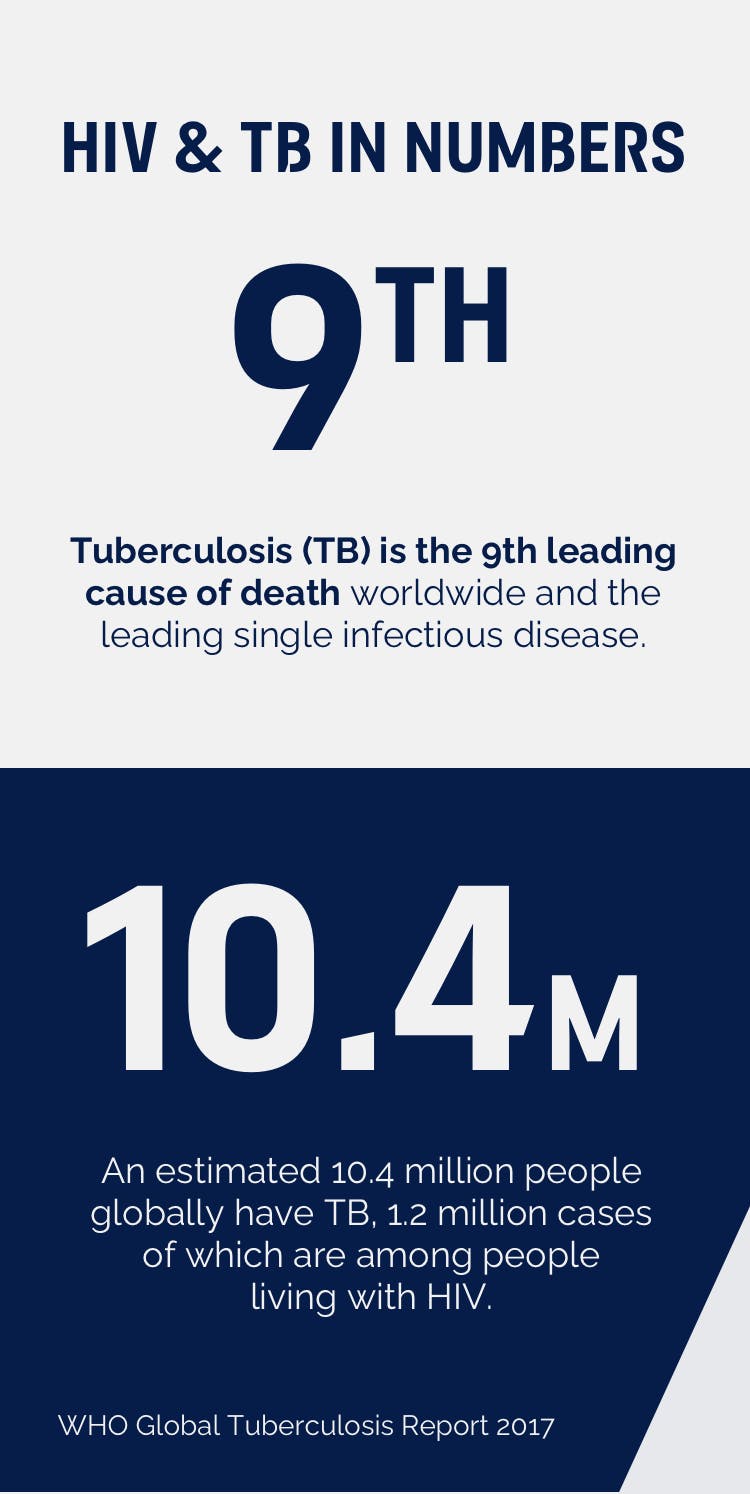
Tuberculosis is the ninth leading cause of death worldwide and the leading single infectious disease globally. There are an estimated 10.4 million people globally who have TB, and 1.2 million are also people living with HIV.3
As with HIV, TB disproportionately affects specific populations and is most prevalent in low-income countries. Almost three-quarters (74%) of people living with HIV, who are also co-infected with TB, reside in Africa. Not only this, but the region also has the highest gap in testing for TB in PLHIV and the provision of treatment.3


The challenge of treating HIV/TB co-infection
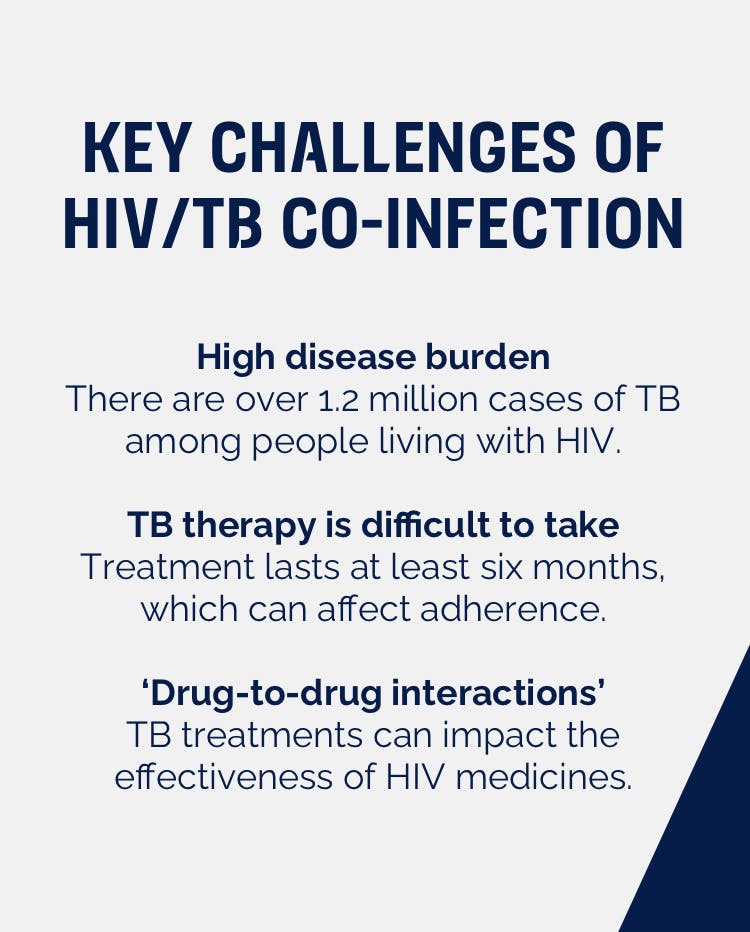
Looking beyond the scale of epidemic and difficulty around testing and diagnosis, there are further challenges facing physicians when they are treating people with both HIV and TB.
Firstly, TB therapy can be quite difficult to take, typically lasting around six months. It’s likely that many of those undergoing the therapy will experience side effects, which cause issues for adherence. In addition to this, many TB therapies will impact the enzymes which metabolise HIV medication. These are known as ‘drug-to-drug interactions’ and need to be carefully managed to ensure effective and safe therapy.
Broadly speaking, when it comes to treating HIV/TB co-infection there are a number of similarities across the two disease areas:
- Effective testing and treatment are limited by logistics and service delivery; this gap leads to delayed testing and late treatment and is most common in low-income countries
- Drug-drug interactions, resistance, toxicity and treatment failure are complex challenges that need addressing
- There is a low uptake of preventive measures

Striving for solutions
Looking to the future, there are a number of focus areas that can help improve the global response to the issue of HIV/TB co-infection:
- Improve our understanding of ways that can help to reduce the spread of the infections – this is important across both HIV and TB as individual therapy areas.
- Identify improvements in diagnosis and testing, especially in low-income countries, to ensure that cases of both HIV and TB are identified earlier.
- Expand use of preventive measures, including treatment as prevention and collaborative HIV/TB treatment and prevention programmes that raise awareness and education within at-risk communities.
- Ensure better access to effective and well-tolerated treatments for HIV/TB co-infected adults – which can only be done through bold and pioneering partnerships.
Tackling the issue of HIV/TB coinfection is a sizeable challenge facing the scientific community and one that must be overcome if we are to end HIV. As ViiV Healthcare – a company 100% dedicated to fighting HIV - we are working in partnership across research partners, patient organisations and community-based organisations to ensure no person living with HIV is left behind.
References
- UNAIDS. Fact sheet
- Avert. Global Tuberculosis Report 2017: A push for multi-sectoral action
- WHO. Global Tuberculosis Report 2017
YOU MAY ALSO BE INTERESTED IN:
We’ve got more than 50 active collaborations worldwide with pharmaceutical and biotechnology companies, government agencies, academic institutions and not-for-profit organisations to broaden our capabilities and enhance our performance.
Incredible advances have been made in the development of effective HIV treatments that allow people living with HIV to suppress their virus to undetectable levels and avoid transmitting it to others. Find out about our approach to HIV cure.
The process of identifying, creating and developing generally well-tolerated and effective innovative HIV therapies is complex and requires ongoing collaboration between research teams that work in many different areas of medicines development.
NP-GBL-HVX-WCNT-230030
If you get any side effects, talk to your doctor, pharmacist or nurse. This includes any possible side effects not listed in the package leaflet. You can also report side effects directly via the Yellow Card Scheme at www.mhra.gov.uk/yellowcard or search for MHRA Yellowcard in the Google Play or Apple App store. By reporting side effects, you can help provide more information on the safety of this medicine.
If you are from outside the UK, you can report adverse events to GSK/ViiV by selecting your region and market, here.


