HIV RESEARCH
When considering the heritage from our founding companies, we can proudly say that we have been involved in the development of effective treatments for HIV/AIDS from the beginning.
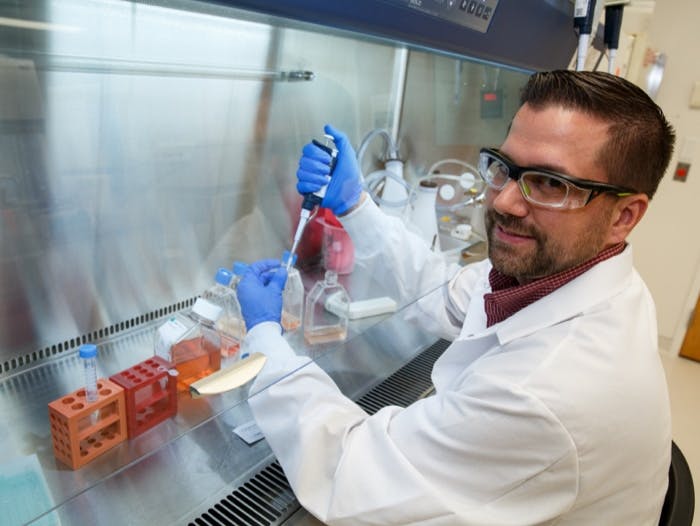
Our scientists and researchers are dedicated to discovering innovative new approaches to improve outcomes for people living with HIV. We are committed to treating, preventing and hopefully one day, curing HIV.
Find out all about current HIV clinical trials and studies, why diversity is important in clinical trials, how they’re regulated and how to get involved.
The needs of people living with HIV change over time, and we‘re exploring new ways of treating and preventing HIV through new mechanisms of action and drug delivery.
The process of identifying, creating and developing generally well-tolerated and effective innovative HIV therapies is complex and requires ongoing collaboration between research teams that work in many different areas of medicines development.
OUR STORIES: SCIENCE AND INNOVATION
Discover how we work with leading researchers and academic groups to innovate and bring the best science to HIV treatment, prevention and care...
To lift the substantial burdens of daily treatment and social stigma associated with HIV, a cure is essential towards accomplishing our goal of ending the HIV epidemic. With this goal in mind, we are in pursuit of a cure for HIV.
We’ve got more than 50 active collaborations worldwide with pharmaceutical and biotechnology companies, government agencies, academic institutions and not-for-profit organisations to broaden our capabilities and enhance our performance.
With significant progress made in the fight against HIV, how do we make sure that clinically proven tools are implemented into real-world settings?
NP-GBL-HVX-COCO-220018 January 2024
If you get any side effects, talk to your doctor, pharmacist or nurse. This includes any possible side effects not listed in the package leaflet. You can also report side effects directly via the Yellow Card Scheme at www.mhra.gov.uk/yellowcard or search for MHRA Yellowcard in the Google Play or Apple App store. By reporting side effects, you can help provide more information on the safety of this medicine.
If you are from outside the UK, you can report adverse events to GSK/ViiV by selecting your region and market, here.