UNDERSTANDING THE HIV EPIDEMIC IN LATIN AMERICA

HIV may not be the first thing that comes to mind when you think about Latin America, but together with the Caribbean, the region is home to an estimated 2.1 million people living with HIV. – that’s almost as many as Western & Central Europe and North America combined.1
Look beyond the numbers and you’ll find a diverse patchwork of different cultures and communities, each with its own unique opportunities and challenges.
Over the past decade, the region has been making progress in fighting the HIV epidemic, with most countries achieving 70-90% towards the UNAIDS 90-90-90 targets. This progress is encouraging but we know there is still more work to be done.
Don’t forget the new kids on the block
Across Latin America and the Caribbean, there is a new generation for whom HIV has not been – and will hopefully never be – top of mind. While this is, of course, a good thing for which we should all be thankful, it comes with risks.
Yes, there are no newspaper headlines or TV bulletins of high-profile deaths from AIDS-related illness, but that doesn’t mean there is no threat. Because of this, we’re actually seeing an increase in HIV prevalence among 18-24 year olds in the region.
Dwindling education and awareness, along with governments’ shifting health priorities away from HIV, puts us at risk of breathing new life into the number of new infections across the region; which have remained steady in recent years.2
The virus and the stigma: a two-pronged attack
The last thirty years of scientific advances transformed HIV diagnoses: conversations which used to be deemed a death sentence are now focussing on managing HIV as a long-term chronic condition.
This looks set to be the new status quo until the discovery of an HIV cure – which remains the end goal for the global medical and research community. In the meantime, we must do all we can to continuously innovate and improve quality of life for people living with HIV – which includes tackling the prevalence of the stigma and discrimination.
Speaking to physicians across the region, we are still seeing a trend of late-presenting patients – namely due to delayed diagnosis driven by the fear and anticipated stigma associated with getting tested and knowing your status.
In at least half the countries in the region, one in three people had a CD4 count under 200 when tested for the first time –3 which is so low that they are considered to have AIDS.4
For communities, but also physicians, we must continue to challenge the misinformation and discrimination around HIV, which is holding us back in our response to the epidemic.
"We must continue to challenge the misinformation and discrimination around HIV, which is holding us back in our response to the epidemic."
HIV is a virus that thrives on inequality
If we are to truly end the epidemic, it is crucial that we ensure that no one person, group or community living with or affected by HIV is left behind.
Our response must reach those groups most at-risk of HIV and address the underlying inequality which creates a fertile environment for both HIV infection and the associated stigma to spread. Across the region there are a number of notable groups who are considered at heightened risk of HIV. These include:
- Men who have sex with men (MSM) are the largest percentage of people in Latin America infected with HIV. Homophobia is common in Latin America, and this prevents activism in many countries in the region.
- HIV transmission is common among sex workers and their patrons and there are higher rates of HIV among street sex-workers. In countries like Bolivia and Ecuador, there are lower rates of infection among this population because of condom use and STI testing check-ups, however this is not the norm across the region.
- Transgender women are highly affected by HIV in Latin America and the Caribbean. HIV prevalence among this group is thought to be 49 times higher than among the general population (ref: UNAIDS (2014) 'The Gap Report 2014')
- Intravenous drug users (IVDU) are often infected with HIV. Argentina, Brazil, Uruguay, and Paraguay are countries where intravenous drug use is a common cause of the spread of HIV. Brazil has seen success with a needle exchange programme that lowered the prevalence of HIV among injecting drug users.
- HIV infection is high among migrant populations in Latin America who move from country to country because of poverty and violence in their home countries. This is currently seriously affecting the migrant population from Venezuela.
Driving access to medicines
One of the great successes across Latin America and the Caribbean in the last decade has been the drive to increase access to universal antiretroviral therapy.
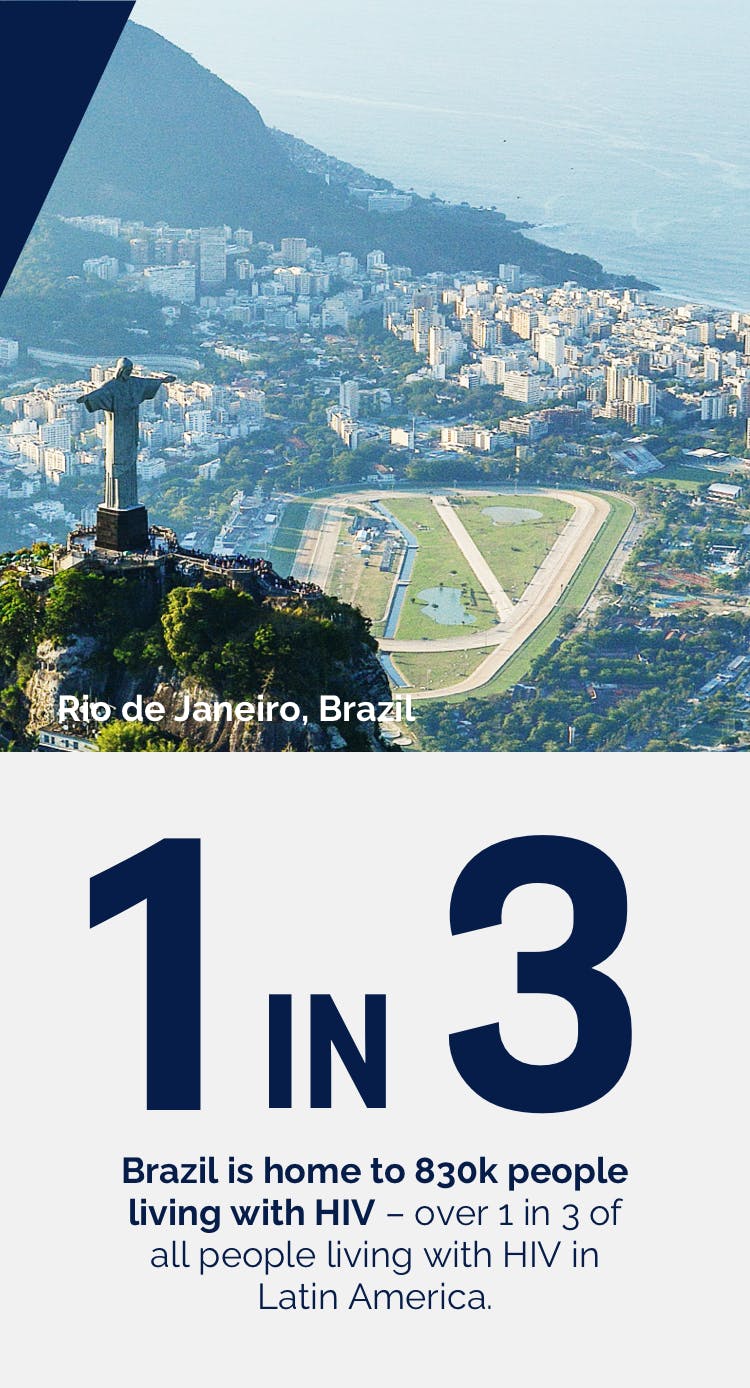
Countries like Brazil have seen health ministries roll out initiatives to utilise treatment as prevention (PrEP) as well ensuring access to innovative ARVs through public-private partnerships, of which ViiV’s was one of the largest schemes. Brazil is home to around 830,000 people living with HIV – almost a third of all those living with HIV across the region.
Providing access to this new generation of innovative medicine, often integrase inhibitors which would typically only be used in cases of resistance or highly treatment experience patients has seen AIDS-related deaths drop significantly.5

What’s next: the future of the HIV response in Latin America?
It’s clear that there’s no ‘silver bullet’ to end the HIV epidemic and that there’s still work to do at an individual, community, national and even supra-national level; but we must stay resilient and committed to delivering an HIV free future.
By supporting at-risk communities, guarding against complacency and continuing to partner – all with a large dose of compassion and understanding – we can make it a reality. I believe, looking at the current state of play, there are a few obvious next steps:
- We should continue to increase harm-reduction programmes, condom access and educational campaigns that are essential to help prevent HIV from spreading.
- Access to stigma-free HIV testing is paramount to diagnosing infected individuals early.
- Foreign aid is needed to help improve healthcare infrastructures to facilitate early diagnosis and treatment.
- Continuing focus from governments to tackle the epidemic; partnered with ongoing, quality conversations between HCPs and their patients that optimise the treatment and care for people living with HIV.
Underlying this, there is a pressing need for better quality data on a number of key populations and for national strategic information systems to be strengthened to make sure that progress is effectively monitored; negative trends are quickly spotted and addressed; and that we have the information we need to continue to address all the challenges of the HIV epidemic.
- https://www.avert.org/global-hiv-and-aids-statistics
- https://www.unaids.org/en/regionscountries/countries/brazil
- https://www.unaids.org/en/regionscountries/countries/
- https://www.unaids.org/sites/default/files/media_asset/undetectable-untransmittable_en.pdf
- https://www.unaids.org/en/regionscountries/countries/brazil
If you get any side effects, talk to your doctor, pharmacist or nurse. This includes any possible side effects not listed in the package leaflet. You can also report side effects directly via the Yellow Card Scheme at www.mhra.gov.uk/yellowcard or search for MHRA Yellowcard in the Google Play or Apple App store. By reporting side effects, you can help provide more information on the safety of this medicine.
If you are from outside the UK, you can report adverse events to GSK/ViiV by selecting your region and market, here.