OUR STORIES ON SCIENCE AND INNOVATION
Discover how we work with leading researchers and academic groups to innovate and bring the best science to HIV treatment, prevention and care…
With modern advancements in HIV medicines and care, people living with HIV can live as long as people without. But unfortunately, HIV stigma is still prevalent. That’s why we are using virtual reality to put HCPs in the shoes of people living with HIV.
In this article by Professor José Gatell, he shares his insights on what multidrug-resistance HIV is and his insights on how to manage such a complex condition.
Thanks to advances in science and innovation, people living with HIV have options for effective treatment that mean they can expect to live long and healthy lives. Find out why understanding the needs and wants of people living with HIV is essential.
Discover the importance of representative research for HIV treatment for people living with HIV
Incredible progress has been made over the past four decades of the HIV epidemic. Gone are the “bad old days” of the epidemic when HIV was the leading cause of death for adults in the US between the ages of 25-44.
You don’t need a PhD to get in on the science with us! For too long, the latest in HIV research and science was limited to laboratories and medical congresses – far away from the lives of the people it impacted the most. With ViiV Healthcare’s Science on the Sofa, we’re changing how we talk about HIV science by breaking down complex concepts in a new way to make the science accessible for everyone.
Find out more about our partnership program which aims to identify and examine predictors and pathways of disease that are specific to people living with HIV.
Dr Harmony Garges, Chief Medical Officer at ViiV Healthcare as she reflects on the discussions at AIDS 2022 and aging with HIV.
Real-World Evidence is an increasingly important aspect of data-driven science, but how can it be utilised to benefit the HIV community?
To lift the substantial burdens of daily treatment and social stigma associated with HIV, a cure is essential towards accomplishing our goal of ending the HIV epidemic. With this goal in mind, we are in pursuit of a cure for HIV.
We’ve got more than 50 active collaborations worldwide with pharmaceutical and biotechnology companies, government agencies, academic institutions and not-for-profit organisations to broaden our capabilities and enhance our performance.
With significant progress made in the fight against HIV, how do we make sure that clinically proven tools are implemented into real-world settings?
Women make up more than half of all people living with HIV – why are they under represented in studies of new medicines?
Collaboration is the key to finding the solutions to HIV challenges – and it’s at the heart of what we do at our HIV research facility in Branford, Connecticut, USA.
Advances in treatment have dramatically improved the life expectancy of people living with HIV (PLHIV), which is welcome progress. However, challenges remain for those ageing with HIV.
Antibodies play a critical role in the immune system’s defence against infection and disease. Broadly neutralising antibodies (bNAbs) are a type of antibody that can recognise and block the entry of a broad range of different strains of HIV into healthy cells.
Kimberly Smith, Head of R&D at ViiV Healthcare, demands the scientific community to drive for the inclusion of more women in HIV clinical trials.
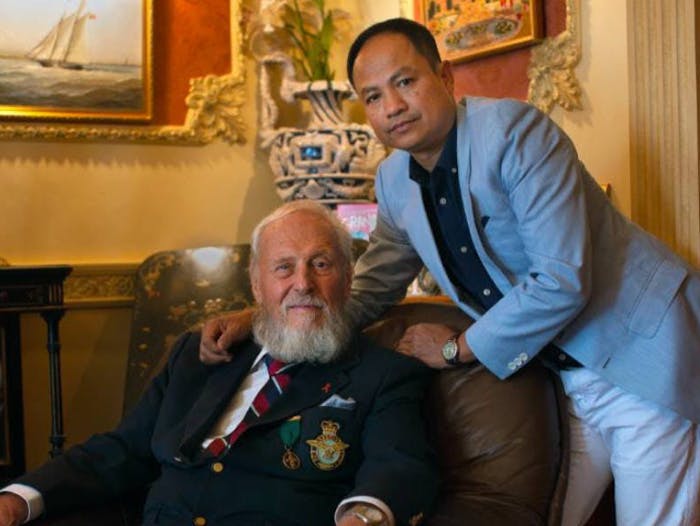
Dr Ben Young, Head of the Global Medical Directors at ViiV Healthcare shares his experience on the impact of COVID-19 on medical conferences.
Dr Benjamin Young, Head, Global Medical Directors at ViiV Healthcare reflects on the last two years of virtual conferences.
EXPLORE OTHER STORIES ON:
Explore our work with NGOs, HCPs, regulatory authorities, HIV clinics and the wider medical community to help ensure people living with HIV get the most effective care globally.
Find out how we're partnering with communities across the world to fight HIV stigma and support people living with HIV.
Read about the experiences of people living with HIV with explanation and segmentation of data from the Positive Perspectives - Waves 1 and 2 studies. Positive Perspectives is one of the largest, global, HIV patient-reported outcomes studies to date.
NP-GBL-HVX-COCO-230017 | March 2024
If you get any side effects, talk to your doctor, pharmacist or nurse. This includes any possible side effects not listed in the package leaflet. You can also report side effects directly via the Yellow Card Scheme at www.mhra.gov.uk/yellowcard or search for MHRA Yellowcard in the Google Play or Apple App store. By reporting side effects, you can help provide more information on the safety of this medicine.
If you are from outside the UK, you can report adverse events to GSK/ViiV by selecting your region and market, here.